The connection between biology and behavior is shaping a new era in mental health. The days of treating psychiatric symptoms without a full understanding of the body’s underlying mechanisms are fading. Now, insights from neuroscience, genetics, and endocrinology are transforming how professionals approach mental well-being. Every mood, decision, or thought is influenced by chemical and structural processes within the body, and mapping those relationships gives clinicians more clarity on why conditions develop and how to treat them effectively.
This evolving understanding has practical outcomes. Grounding psychiatric care in biology enables professionals to better predict which interventions will work, monitor changes more precisely, and measure recovery in tangible ways.
Applying Neurobiological Insights
Neurobiology provides a framework for understanding the physical basis of behavior. When clinicians examine how brain structures communicate or how neurons respond to stimuli, they gain a clearer picture of why certain patterns of emotion or thought emerge. This understanding refines every layer of psychiatric care, from diagnosis to medication management to therapy planning. Incorporating data from brain imaging, electrophysiological studies, and neurotransmitter research, treatment moves away from generalizations and becomes targeted, measurable, and adaptive. Such findings prove valuable for almost all professionals in a healthcare setting, whether a psychiatric nurse or a general psychiatrist.
Both the psychiatrist and the psychiatric nurse practitioner play vital roles in applying these insights. A psychiatrist may focus on the neurochemical pathways behind a disorder and use imaging or medication to modify them, while a nurse practitioner can integrate biological understanding into therapy, monitoring, and long-term support. The discussion around psychiatrist vs PMHNP is not about hierarchy but about perspective, as each role brings different strengths in translating science into patient progress. Together, they form a collaborative model of care that uses biology not as a theory but as a daily tool for better outcomes.
Exploring Neurotransmitter Activity
Neurotransmitters are the language of the brain, carrying signals that shape everything from attention and motivation to anxiety and rest. Studying how these chemicals, serotonin, dopamine, GABA, and others, interact helps clinicians design more effective treatment plans. For example, understanding dopamine dysregulation allows for precision in addressing conditions like schizophrenia or ADHD, while serotonin mapping informs decisions around antidepressant selection.
Advancements in pharmacogenomics have also made it possible to predict how a person’s genetic makeup influences their response to certain medications. This reduces the trial-and-error approach that has long been part of psychiatry.
Examining the Gut-Brain Connection
The link between gut health and mental well-being has become one of the most compelling developments in biological psychiatry. The microbiome, which is the vast network of bacteria in the digestive system, produces neurotransmitters, regulates inflammation, and communicates directly with the brain through the vagus nerve. When the gut’s balance shifts, mood and cognition often shift too. This relationship has prompted many psychiatric professionals to consider nutrition and digestive health as central elements of emotional stability.
Research now supports the use of probiotics, prebiotics, and diet adjustments to support mental health treatment. A balanced gut environment can influence serotonin production, reduce anxiety, and improve energy regulation. For patients with chronic stress or depression, small biological interventions, like restoring gut balance, can work alongside therapy or medication to enhance overall outcomes.
Identifying Predictive Biomarkers
Biomarkers give psychiatry something it has long needed: measurable signals that forecast changes in mental health. These markers can include hormones, inflammatory molecules, genetic patterns, or brain activity signatures that point to risk or resilience. When clinicians identify them early, they can act before symptoms return or escalate.
Tracking biomarkers allows clinicians to tailor interventions precisely. For example, if inflammation markers rise, adjustments can be made before a depressive episode begins. If hormone levels or sleep patterns shift, medication or therapy can adapt accordingly.
Linking Hormonal Balance and Emotion
Hormones form an invisible network that influences mood, energy, and motivation. Subtle imbalances in cortisol, estrogen, or thyroid hormones can alter how patients think and feel, often mimicking or intensifying psychiatric symptoms.
Monitoring hormonal activity allows clinicians to support more complete recovery plans. Collaboration between endocrinologists and mental health providers ensures that treatment focuses on both the physical and psychological aspects of imbalance.
Studying Inflammation in Psychiatry
Inflammation plays a significant role in the way mental health conditions develop and progress. Research continues to show that inflammatory molecules can influence mood regulation, energy levels, and cognition. Chronic low-grade inflammation may alter neurotransmitter function, contributing to conditions such as depression, anxiety, and fatigue. Understanding this link allows clinicians to view psychiatric disorders through a wider biological lens, recognizing that the immune system and the brain are in constant communication.
Modern psychiatric care is beginning to incorporate inflammation monitoring into patient assessments. Anti-inflammatory treatments, dietary adjustments, and exercise routines that lower inflammatory markers are being explored as complementary approaches. This biological awareness helps clinicians shape care that doesn’t rely on medication alone but instead treats the root systems influencing mental well-being.
Using Biological Feedback
Biological feedback tools bridge science and therapy in real time. Systems like EEG, heart rate variability tracking, and skin conductance monitoring reveal how the body responds to thought and emotion. Such insights allow patients to see their reactions instead of guessing them, turning awareness into skill. With this information, therapy becomes more interactive and personalized, building self-regulation through observation and practice.
Biofeedback also strengthens the relationship between patients and their bodies. When individuals learn to influence physical patterns, slowing their heart rate or reducing tension, they develop confidence in their ability to manage stress. Clinicians use biological cues as training points for attention, focus, and calmness.
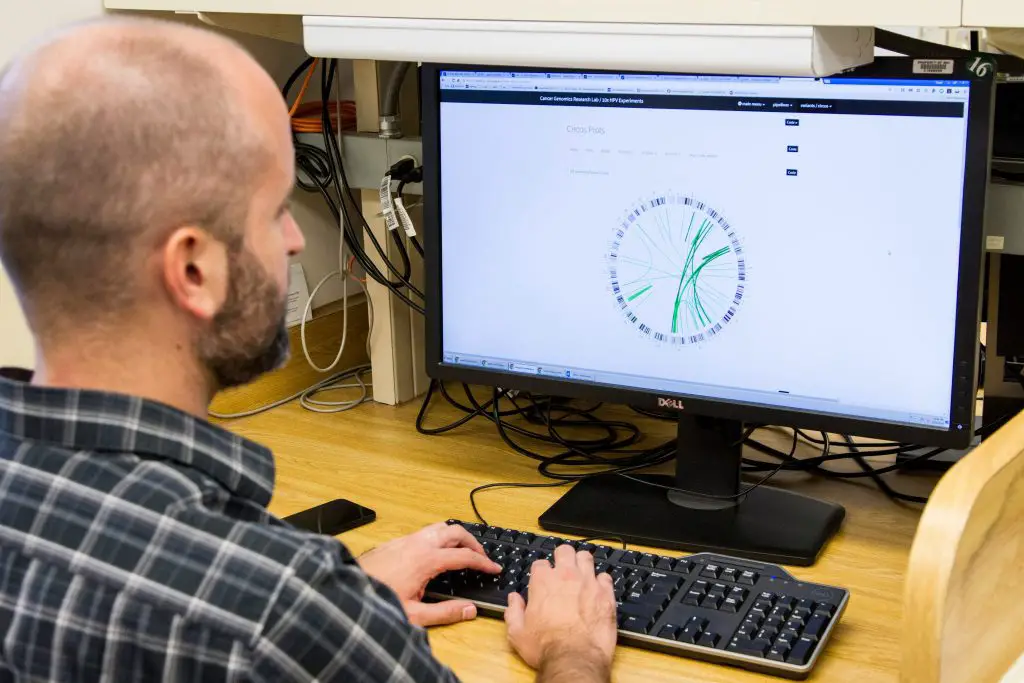
Training Clinicians in Data Interpretation
The integration of biological data into psychiatry demands new forms of training. Clinicians must learn how to interpret genetic, hormonal, and neurological information with accuracy and empathy. This knowledge ensures that biological markers inform decisions rather than overwhelm them. Education that connects biology with behavior helps professionals translate complex findings into practical guidance for patients.
Interdisciplinary learning between psychiatry, neuroscience, and internal medicine supports this effort. When professionals understand both the science and the lived experience of mental health, care becomes unified and more effective. Interpreting biological data accurately ensures that science enhances human understanding instead of distancing it.
Biological knowledge gives psychiatry the depth it has long needed. It replaces guesswork with measurable understanding and transforms treatment from symptom management to true insight. Each area, like neurobiology, hormones, neurotransmitters, inflammation, and stress, adds clarity to the complex story of how the body and mind influence one another. This approach builds trust between patients and professionals because decisions are grounded in evidence that patients can see and understand.