The Future of Healthcare
As the world continues to face major health shifts—aging populations, long-term effects of COVID-19, mental health crises, and a chronic staffing shortage—one thing is clear. Machines can help. AI can predict. Apps can track. But they can’t feel your pulse and know something’s off. They can’t explain a diagnosis in a way that makes it less terrifying. And they definitely can’t offer real-time judgment in a chaotic trauma unit.
Behind every high-tech solution is a human being making the call, catching what others missed, or just being the calm in someone’s worst moment. Right now, the gap between patient needs and professional supply is growing fast. And it’s putting a spotlight on something that can’t be automated: skill.
In this blog, we will share why the future of healthcare depends on skilled professionals, and how we’re all going to feel the difference when they’re supported—or when they’re not.
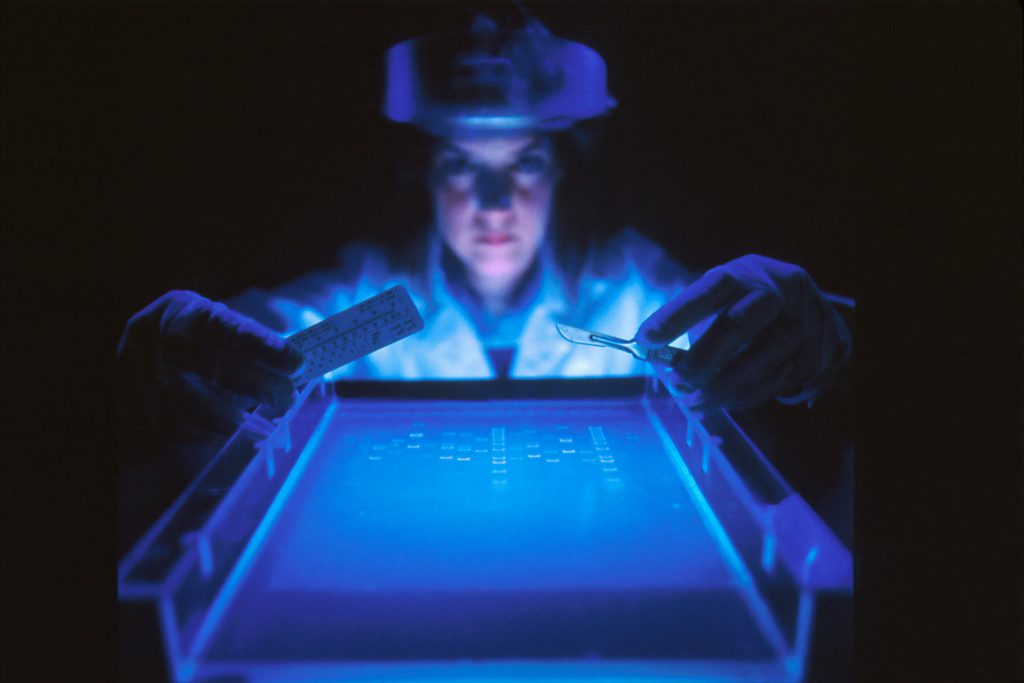
Training, Not Tech, Will Define Healthcare’s Next Era
There’s no denying it. Tech is transforming healthcare. AI can read scans. Robots assist in surgeries. Smartwatches send heart data straight to the cloud. The tools are impressive. But they’re still just tools. And tools don’t matter much without someone trained to use them well.
What’s often left out of the shiny narrative is the essential role of the human behind the screen. A CT scanner doesn’t diagnose. A blood pressure cuff doesn’t interpret the result. Skilled professionals take the data and turn it into action.
That’s where education and advanced training come in. It’s not enough to just be present in the room. Today’s healthcare workers need sharper clinical judgment, better communication skills, and the ability to collaborate across complex systems. For nurses, one of the most popular paths to deepen those skills is the RN to BSN program. It’s designed for registered nurses who want to level up their knowledge and improve patient outcomes. The program focuses on leadership, critical thinking, community health, and evidence-based care.
Hospitals are taking note. Many are giving hiring priority—and better pay—to BSN-prepared nurses. Not because it looks good on paper, but because they perform better in high-pressure environments. They understand how to connect daily practice to broader trends. They take part in decision-making, not just task completion.
As care becomes more complex, these upgraded skill sets aren’t just helpful. They’re non-negotiable.
The Skills Shortage Isn’t Coming. It’s Here.
The pandemic didn’t create the shortage. It just ripped the cover off it. Burnout spiked. Early retirements rolled in. And now the industry is scrambling to fill gaps that were already growing. According to the U.S. Bureau of Labor Statistics, healthcare is expected to add over two million jobs in the next decade. That sounds like a win until you realize we don’t yet have enough trained professionals to meet that demand.
This shortage doesn’t just affect hospitals. It trickles down to schools, clinics, nursing homes, home care, and rural health centers. Delays in treatment. Shorter appointments. Less time with patients. More room for error.
And here’s the twist: people are living longer. Which means they need more care, for more conditions, over more years. Aging populations don’t just bring more patients. They bring more complicated care plans. More meds. More monitoring. More moments where the skill of a provider can literally change the outcome.
Skilled professionals don’t just help the system run smoothly. They are the system.
Soft Skills Matter More Than Ever
Let’s talk about something that doesn’t show up on resumes but shows up in every patient interaction: people skills. Clinical skill can save a life. But emotional intelligence can save a person’s experience of their life.
Healthcare is shifting toward whole-person care. It’s no longer enough to treat the disease. Patients want to feel heard. Understood. Respected. That means professionals need more than technical knowledge. They need empathy. Cultural sensitivity. The ability to explain, de-escalate, and sometimes just sit with someone in silence.
These skills can’t be faked. And they definitely can’t be programmed. But they can be taught and strengthened. That’s why more training programs are folding communication, ethics, and collaboration into their curriculums. That’s also why healthcare systems are investing in wellness and support for their staff. Because people who feel burned out aren’t likely to offer comfort to someone else.
In short, the soft stuff? It’s becoming core.
A More Diverse Workforce Means Better Care
The makeup of the healthcare workforce should reflect the communities it serves. And right now, it doesn’t. That disconnect can lead to mistrust, misunderstandings, and worse outcomes.
Studies have shown that when patients are treated by professionals who understand their background, their care improves. They’re more likely to follow instructions. They report better experiences. They’re more likely to come back when they need help again.
Creating a more diverse healthcare workforce takes more than just good intentions. It takes access to education, mentorship, and pathways for growth. Programs that support underrepresented students through medical or nursing school aren’t just about fairness. They’re about smarter systems.
Because better care isn’t just about what’s done. It’s also about who’s doing it.
Technology Can’t Replace Judgment
AI might be able to spot a tumor faster than the human eye. But it doesn’t know your history. It doesn’t understand your hesitation. It doesn’t notice when your tone shifts or when something feels “off” even if your chart looks fine.
Only trained professionals can do that.
Machines can process. Humans can perceive. That distinction matters more than ever in complex care environments. It’s why medical errors still happen, even with all the tech in the world. Because it’s not just about having data. It’s about interpreting it, responding to it, and connecting it to real human needs.
That’s where skill makes the difference. Not just technical ability, but the kind of thinking that takes years to develop. Judgment that comes from experience. Knowing when to follow the protocol and when to ask more questions. That kind of decision-making isn’t built into a device. It’s built into people.
The bottom line? Healthcare only works when its people are trained, supported, and valued. Gadgets help, but it’s skilled professionals who keep the system running. The future depends on how we train, retain, and uplift them. Patients might not see the effort behind the care, but they’ll always feel its presence—or its absence. The core of healthcare is, and always will be, human.